Findings of Abdominal Computed Tomography In COVID-19 Patients with Abnormal Abdominal Symptoms In Siriraj Hospital
DOI:
https://doi.org/10.46475/asean-jr.v25i2.886Keywords:
Abdominal imaging, Abdominal symptoms, COVID-19, Corona- virusAbstract
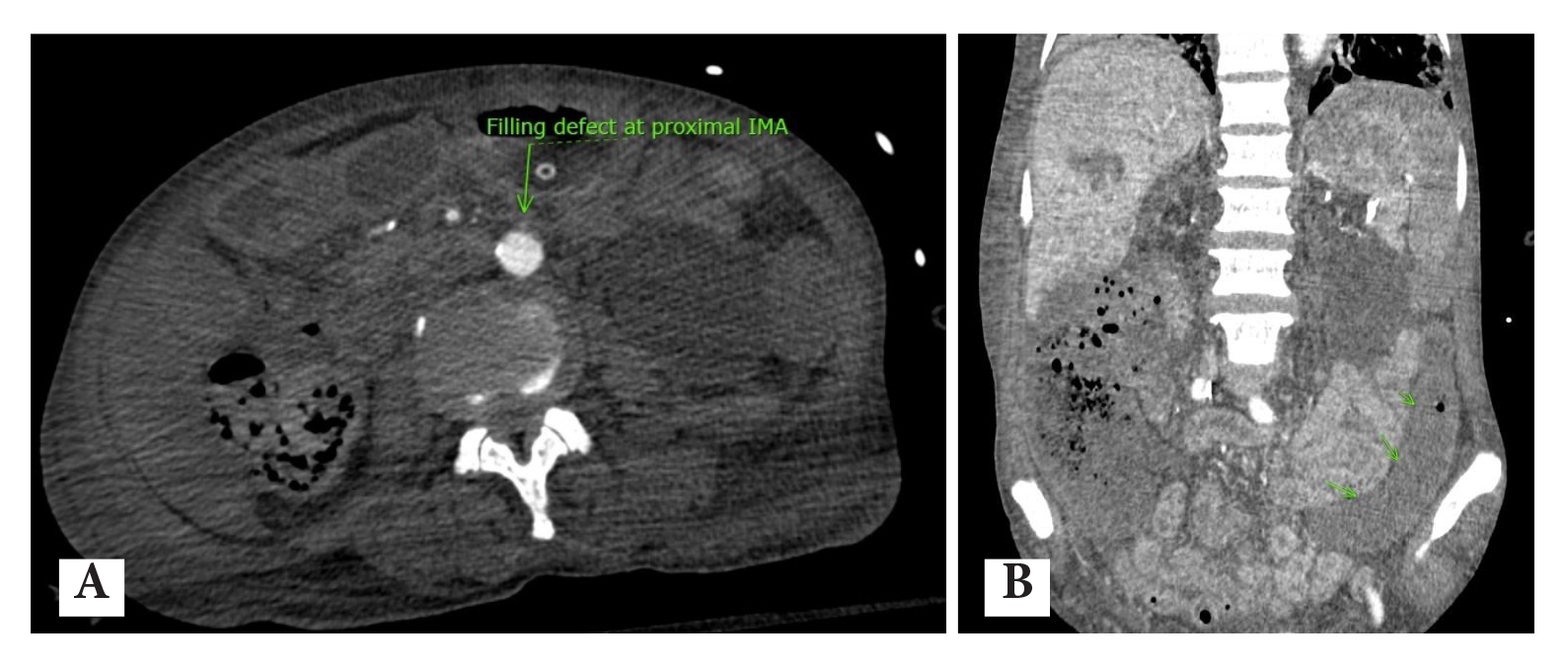
Background: The coronavirus (COVID-19) is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Chest imaging findings of COVID-19 disease have been widely published. Only a few studies of abdominal imaging findings have been documented. The majority of these studies demonstrate thrombotic events associated with COVID-19. Previous studies were mainly conducted in the USA, Europe and China which limited the applicability in Southeast Asia (SEA) including Thailand.
Objective: To provide a summary of various abdominal imaging findings of COVID-19 patients admitted to xxx Hospital with findings associated with clinical outcomes.
Materials and Methods: All CT abdominal imaging of adult patients who tested positive for COVID-19 performed from January 1st, 2020 to August 31st, 2022 were retrospectively reviewed. We collected clinical data, abdominal signs and symptoms, laboratory data and various CT findings, for example; bowel-wall thickening, bowel ischemia, fluid-filled colon and bleeding manifestations. The clinical outcomes were gathered as death confirmation, invasive mechanical ventilation, days of invasive mechanical ventilation and days of hospitalization.
Results: A large number of patients who had stage 3-5 chronic kidney disease (CKD), abdominal distension, abnormal bowel findings and longer days of hospitalization were significantly observed in a group with worse clinical outcomes. Abnormal intestinal imaging findings were related to a higher risk of worse outcomes, invasive mechanical ventilation, death and days of hospitalization without statistical significance.
Conclusion: Abdominal CT scans performed on COVID-19 patients frequently revealed abnormal bowel findings, which were strongly associated with poor clinical outcomes. Radiologists need to be concerned about abnormal bowel findings and point them out to clinicians and surgeons.
Downloads
Metrics
References
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. lancet 2020;395:497-506. doi: 10.1016/S0140-6736(20)30183-5. DOI: https://doi.org/10.1016/S0140-6736(20)30183-5
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708-20. doi: 10.1056/NEJMoa2002032. DOI: https://doi.org/10.1056/NEJMoa2002032
Johns Hopkins coronavirus resource center [Internet]. Baltimore (MD) :Johns Hopkins University & Medicine; c2024 [cited 2024 Jun 8]. Available from: https://coronavirus.jhu.edu/about .
Cheung KS, Hung IFN, Chan PPY, Lung K, Tso E, Liu R, et al. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from a Hong Kong cohort: systematic review and meta-analysis. Gastroenterology 2020;159:81-95. doi: 10.1053/j.gastro.2020.03.065. DOI: https://doi.org/10.1053/j.gastro.2020.03.065
Luo S, Zhang X, Xu H. Don't overlook digestive symptoms in patients with 2019 novel coronavirus disease (COVID-19). Clin Gastroenterol Hepatol 2020;18:1636-7. doi: 10.1016/j.cgh.2020.03.043. DOI: https://doi.org/10.1016/j.cgh.2020.03.043
Pan L, Mu M, Yang P, Sun Y, Wang R, Yan J, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol 2020;115:766-73. doi: 10.14309/ajg.0000000000000620. DOI: https://doi.org/10.14309/ajg.0000000000000620
Gu J, Han B, Wang J. COVID-19: gastrointestinal manifestations and potential fecal–oral transmission. Gastroenterology 2020;158:1518-9. doi: 10.1053/j.gastro.2020.02.054. DOI: https://doi.org/10.1053/j.gastro.2020.02.054
Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020;181:271-80.e8. doi: 10.1016/j.cell.2020.02.052. DOI: https://doi.org/10.1016/j.cell.2020.02.052
Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol 2004;203:631-7. doi: 10.1002/path.1570. 10. Harmer D, Gilbert M, Borman R, Clark KL. Quantitative mRNA expression profiling of ACE 2, a novel homologue of angiotensin converting enzyme. FEBS lett 2002;532:107-10. doi: 10.1016/s0014-5793(02)03640-2. DOI: https://doi.org/10.1002/path.1570
Mao R, Liang J, Shen J, Ghosh S, Zhu LR, Yang H, et al. Implications of COVID-19 for patients with pre-existing digestive diseases. Lancet Gastroenterol Hepatol 2020;5:425-7. doi: 10.1016/S2468-1253(20)30076-5. DOI: https://doi.org/10.1016/S2468-1253(20)30076-5
Bhayana R, Som A, Li MD, Carey DE, Anderson MA, Blake MA, et al. Abdominal imaging findings in COVID-19: preliminary observations. Radiology 2020;297:E207. doi: 10.1148/radiol.2020201908. DOI: https://doi.org/10.1148/radiol.2020201908
Gornet JM, Tran Minh MT, Leleu F, Hassid D. What do surgeons need to know about the digestive disorders and paraclinical abnormalities induced by COVID-19? J Visc Surg 2020;157(3 Suppl 1):S51-7. doi: 10.1016/j.jviscsurg.2020.04.017. DOI: https://doi.org/10.1016/j.jviscsurg.2020.04.017
A Beccara L, Pacioni C, Ponton S, Francavilla S, Cuzzoli A. Arterial mesenteric thrombosis as a complication of SARS-CoV-2 infection. Eur J Case Rep Intern Med 2020;7:001690. doi: 10.12890/2020_001690. DOI: https://doi.org/10.12890/2020_001690
Guo Y, Hu X, Yu F, Chen J, Zheng W, Liu J, et al. Abdomen CT findings in a COVID-19 patient with intestinal symptoms and possibly false negative RT-PCR before initial discharge. Quant Imaging Med Surg 2020;10:1158-61. doi: 10.21037/qims-20-463. DOI: https://doi.org/10.21037/qims-20-463
de Barry O, Mekki A, Diffre C, Seror M, El Hajjam M, Carlier RY. Arterial and venous abdominal thrombosis in a 79-year-old woman with COVID-19 pneumonia. Radiol Case Rep 2020;15:1054-7. doi: 10.1016/j.radcr.2020.04.055.. DOI: https://doi.org/10.1016/j.radcr.2020.04.055
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054-62. doi: 10.1016/S0140-6736(20)30566-3. DOI: https://doi.org/10.1016/S0140-6736(20)30566-3
Crawford SE, Ramani S, Blutt SE, Estes MK. Organoids to dissect gastrointestinal virus–hostiInteractions: What have we learned? Viruses 2021;13:999. doi: 10.3390/v13060999. DOI: https://doi.org/10.3390/v13060999
Horvat N, Pinto PVA, Araujo-Filho JAB, Santos JMMM, Dias AB, Miranda JA, et al. Abdominal gastrointestinal imaging findings on computed tomography in patients with COVID-19 and correlation with clinical outcomes. Eur J Radiol Open 2021;8:100326. doi: 10.1016/j.ejro.2021.100326.. DOI: https://doi.org/10.1016/j.ejro.2021.100326
Goldberg-Stein S, Fink A, Paroder V, Kobi M, Yee J, Chernyak V. Abdominopelvic CT findings in patients with novel coronavirus disease 2019 (COVID-19). Abdom Radiol (NY) 2020;45:2613-23. doi: 10.1007/s00261-020-02669-2.
Parry AH, Wani AH, Yaseen M. Acute mesenteric ischemia in severe coronavirus-19 (COVID-19): possible mechanisms and diagnostic pathway. Acad Radiol 2020;27:1190. doi: 10.1016/j.acra.2020.05.016. DOI: https://doi.org/10.1016/j.acra.2020.05.016
Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res 2020;191:9-14. doi: 10.1016/j.thromres.2020.04.024. DOI: https://doi.org/10.1016/j.thromres.2020.04.024
Escher R, Breakey N, Lämmle B. Severe COVID-19 infection associated with endothelial activation. Thromb Res 2020;190:62. doi: 10.1016/j.thromres.2020.04.014. DOI: https://doi.org/10.1016/j.thromres.2020.04.014
Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020;395:1417-8. doi: 10.1016/S0140-6736(20)30937-5. DOI: https://doi.org/10.1016/S0140-6736(20)30937-5
Santos Leite Pessoa M, Franco Costa Lima C, Farias Pimentel AC, Godeiro Costa JC, Bezerra Holanda JL. Multisystemic infarctions in COVID-19: focus on the spleen. Eur J Case Rep Intern Med 2020;7:001747. doi: 10.12890/2020_001747. DOI: https://doi.org/10.12890/2020_001747
Vaidya T, Nanivadekar A, Patel R. Imaging spectrum of abdominal manifestations of COVID-19. World J Radiol 2021 ;13:157-70. doi: 10.4329/wjr.v13.i6.157. DOI: https://doi.org/10.4329/wjr.v13.i6.157
Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 2020;191:145-7. doi: 10.1016/j.thromres.2020.04.013. DOI: https://doi.org/10.1016/j.thromres.2020.04.013
Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 2020;18:844-7. doi: 10.1111/jth.14768. DOI: https://doi.org/10.1111/jth.14768
Al-Samkari H, Karp Leaf RS, Dzik WH, Carlson JCT, Fogerty AE, Waheed A, et al. COVID-19 and coagulation: bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood 2020;136:489-500. doi: 10.1182/blood.2020006520. DOI: https://doi.org/10.1182/blood.2020006520
Mazzitelli M, Serapide F, Tassone B, Laganà D, Trecarichi EM, Torti C. Spontaneous and severe haematomas in patients with COVID-19 on low-molecular-weight heparin for paroxysmal atrial fibrillation. J Hematol Infect Dis 2020 ;12:e2020054. doi: 10.4084/MJHID.2020.054. DOI: https://doi.org/10.4084/mjhid.2020.054
Scialpi M, Russo P, Piane E, Gallo E, Scalera GB. First case of retroperitoneal hematoma in COVID-19. Turk J Urol 2020;46:407-9. doi: 10.5152/tud.2020.20302. DOI: https://doi.org/10.5152/tud.2020.20302
Zhang J, He X, Hu J, Li T. Retroperitoneal hemorrhage during veno-venous extracorporeal membrane oxygenation in COVID-19 patientss: clinical experience and review of literature. Research Square [Internet]. 2024 [cited 2024 Jun 7]. Available from: https://www.researchsquare.com/article/rs-32685/v1
Erdinc B, Raina JS. Spontaneous retroperitoneal bleed coincided with massive acute deep vein thrombosis as initial presentation of COVID-19. Cureus 2020;12:e9772. doi: 10.7759/cureus.9772. DOI: https://doi.org/10.7759/cureus.9772
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 The ASEAN Journal of Radiology

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Disclosure Forms and Copyright Agreements
All authors listed on the manuscript must complete both the electronic copyright agreement. (in the case of acceptance)